Operationalizing Intersectionality Theory in Research
WORKING THROUGH STIGMA
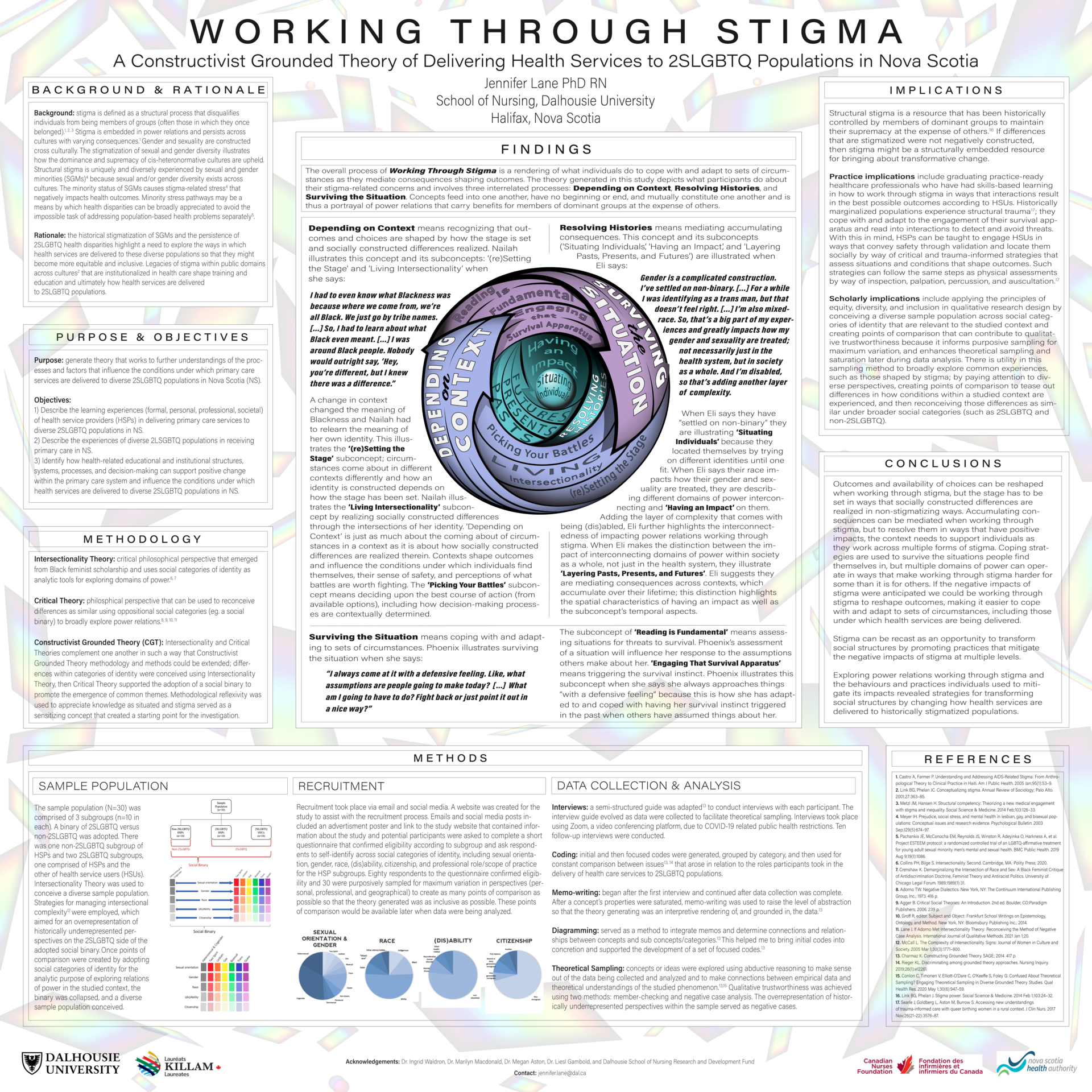
This study was designed to generate theory that works to further understandings of the processes and factors influencing the conditions under which primary care services are delivered to diverse 2SLGBTQ populations in Nova Scotia. This Constructivist Grounded Theory study employed Intersectional and Critical lenses, complicated the notion of identity in a broadly inclusive manner, and gained insight into socio-structural factors that influence access to health services in primary care settings across Nova Scotia. By conducting a preliminary literature review, stigma was identified as significant to the health outcomes of 2SLGBTQ populations, justifying its use as a starting point for the investigation. Upon REB approval, a diverse sample population was recruited; variation was maximized across categories of identity (sexual orientation, gender, race, (dis)ability, and citizenship), geographies, and professional scope of practice/role. Sampling purposively from historically underrepresented groups so they were overrepresented in the sample population created points of comparison for the purpose of enhancing data analysis and generation of a robust grounded theory. The sample population (n=30) was comprised of three subgroups: 2SLGBTQ health service users (HSUs) (n=10), 2SLGBTQ health service providers (HSPs) (n=10), and non-2SLGBTQ HSPs (n=10). Semi-structured interviews lasting up to 90 minutes were conducted with each participant using video-conferencing software. Participants confirmed that stigma was a meaningful construct; its significance was substantiated throughout the data collection process. Conceiving stigma as a socio-structural process that determines health outcomes allowed for an exploration of 2SLGBTQ stigmatization in health care by investigating the delivery of primary care services to 2SLGBTQ populations across a provincial health system. Data analysis started with its collection by way of constant comparison, and continued through coding methods, memo-writing, diagramming, and writing this dissertation. As such, the level of abstraction was raised and a substantive theory of Working Through Stigma was co-created. The main concern of participants was that stigma causes individuals to experience power relations differently and the experiences of those with relatively less power are often disproportionately negative. The theory depicts what participants are doing about their concerns and involves three interrelated processes: depending on context, resolving histories, and surviving the situation.